The Moderating Effect of Practicing Body Psychotherapy

Research shows the disruptive effects of early maltreatment on the autonomic nervous system (ANS) functioning in adulthood. Psychotherapists not only tend to report higher rates of personal experience with early maltreatment, but also fewer mental problems and disturbances in adulthood, as compared to other professions.
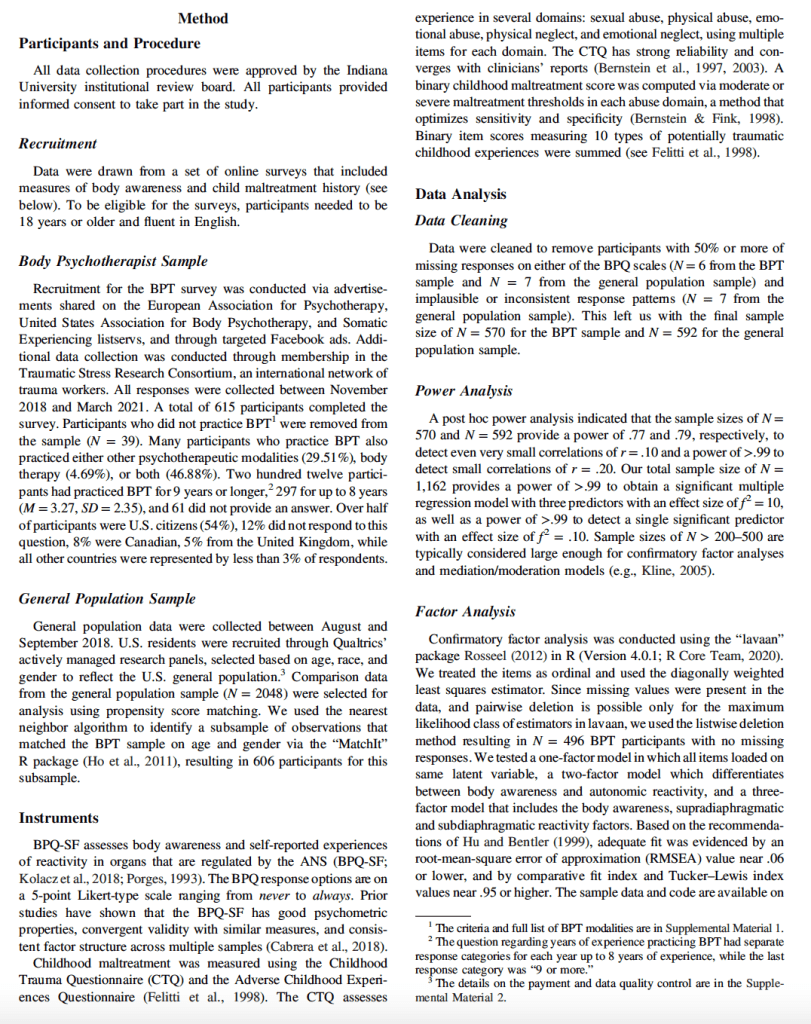
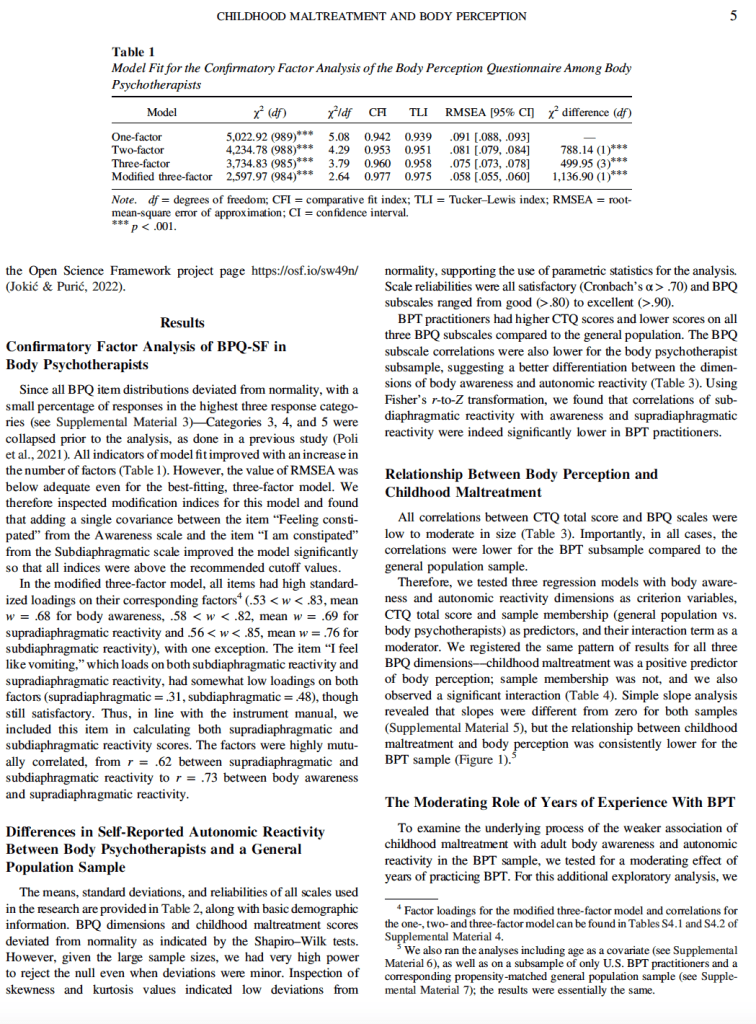
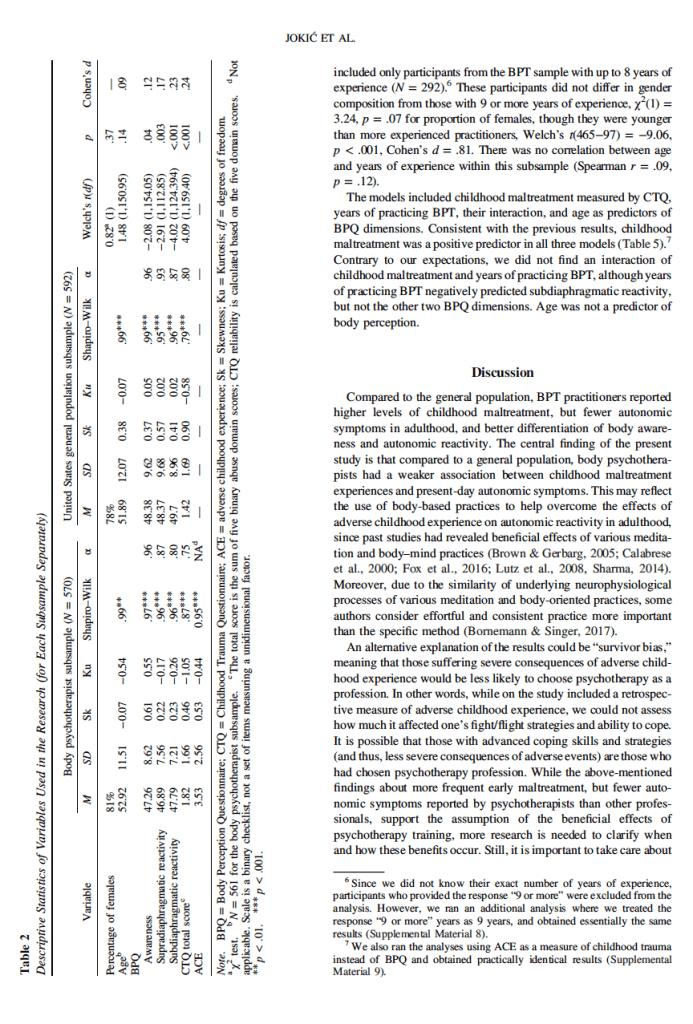
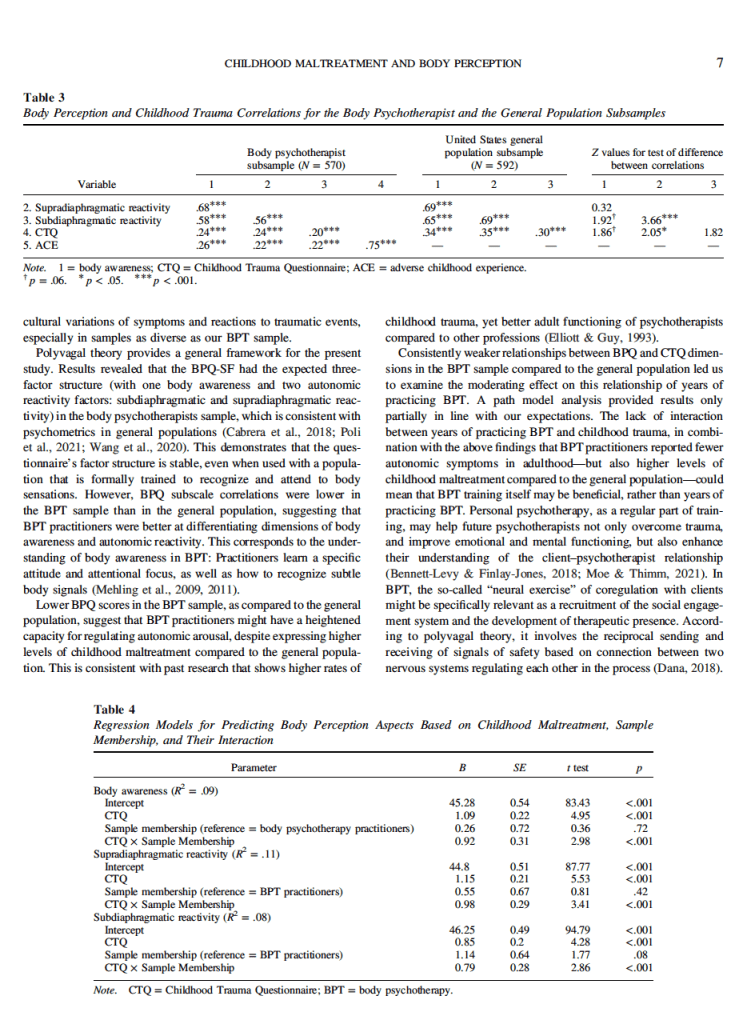
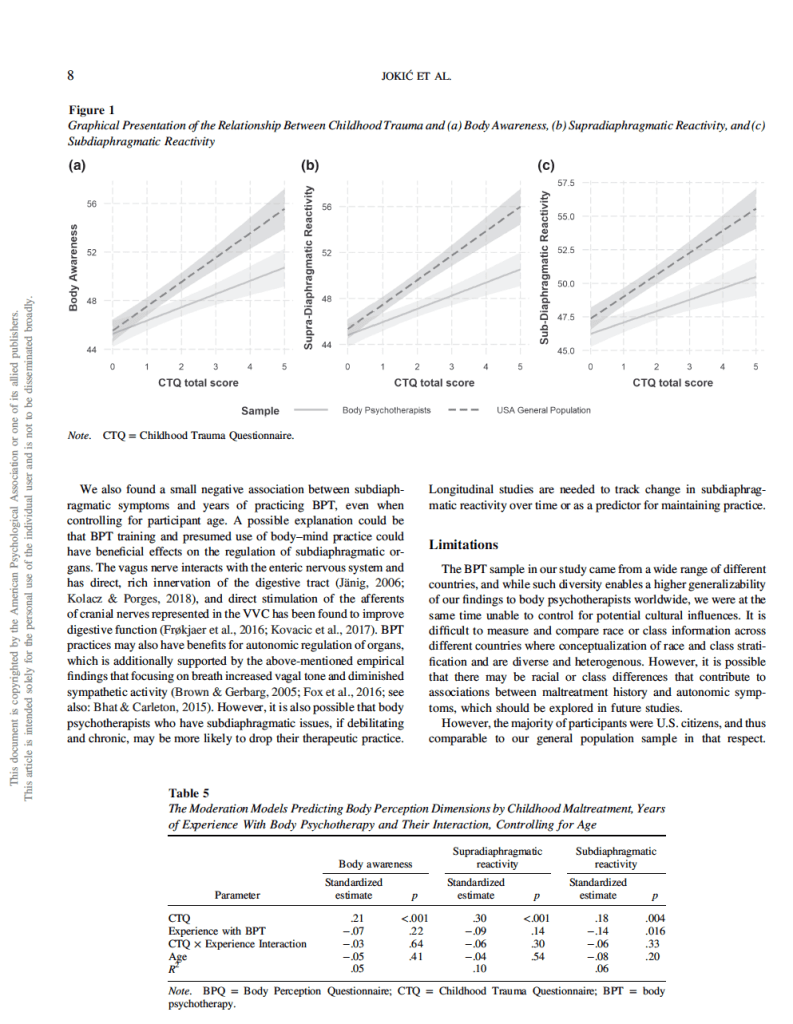
However, the role of the ANS in these processes has been understudied despite the relevance of the therapist’s psychological state and related nonverbal communication for the therapeutic alliance. By comparing body psychotherapists to the general population, the present study aimed to explore the effects of practicing body psychotherapy (BPT) on the link between early maltreatment and autonomic reactivity in adulthood. An online study included 570 body psychotherapists from 35 countries (54% from the United States, Mage = 52.92, 81% of females) and 592 participants from the U.S. general population (Mage = 51.89, 78% females).We first inspected the factorial structure of the Body Perception Questionnaire–Short Form (Cabrera et al., 2018) in the specific population of BPT practitioners, confirming the three-factor model with one body awareness and two autonomic reactivity factors. Compared to the general population, BPT practitioners reported higher levels of childhood maltreatment, but fewer autonomic symptoms in adulthood, better differentiation of body awareness and autonomic reactivity, and a weaker association between childhood maltreatment experiences and present-day autonomic symptoms. Results are discussed in the framework of polyvagal theory.
Early maltreatment impacts not only psychological levels of human functioning (Xiao et al., 2021) but also physiological––in particular, the autonomic nervous system (ANS), shaping behavior and reactions to life events in adulthood (Brindle et al., 2022; Kolacz et al., 2019; McCrory et al., 2011). The disruptive effect of adverse childhood experience has also been recognized in the population of psychotherapists, especially for its impact on emotional burdens (Simionato & Simpson, 2018) and the quality of the therapeutic alliance (Steel et al., 2018). This is particularly relevant since the role of the therapist and the therapeutic alliance have been identified as significant factors in therapy outcome (Baldwin & Imel, 2013; Flückiger et al., 2018; Johns et al., 2019). However, to our knowl-edge, the specific effects of early maltreatment on the ANS func-tioning of psychotherapists have not been studied.
The ANS: The Effects of Childhood Experience. The ANS is a brain–body network that coordinates metabolic processes to support organ function and promotes biobehavioral reactions to danger and anticipated threats (Cannon, 1929; Hess, 1948; Langley, 1921; Porges, 1995; Thayer & Lane, 2000). Recently, the relevance of the ANS for psychological well-being, and especially the parasympathetic nervous system, has been further developed within the framework of polyvagal theory (Porges, 1995, 2011).
Based on evidence from comparative anatomy, neurophysiology, and behavioral research, polyvagal theory (Porges, 1995, 2009, 2011) expands the traditional model of the ANS by elaborating two distinct vagal circuits within the parasympathetic nervous system: a ventral vagal complex (VVC; which is involved in regulating an integrated social engagement system consisting of the striated muscles of the face and head, and the visceral organs above the diaphragm) and a dorsal vagal complex (which in mammals is primarily involved in regulating the organs below the diaphragm).
A key principle of the polyvagal theory is that the structure and function of the ANS emerged as a product of evolution (Porges, 1995). While the early ANS was optimized for threat responses such as mobilization and death feigning, the mammalian ANS integrates autonomic circuits with muscles of the face and head to promote social safety signaling (Porges, 1995, 1998, 2021). This integration of circuits forms a foundation for the social engagement system, which can disengage defense responses and enable affiliative social interactions (Porges, 2021).
Because the ANS is highly responsive to environmental influ-ences and signals of safety and threat, early life maltreatment may disturb safety-related homeostatic functions. Evidence for a causal link between child maltreatment and autonomic regulation has been shown through randomized studies, with interventions that change children’s autonomic activity (Hastings et al., 2019; McLaughlin et al., 2015; Porges et al., 2019). Maladaptive profiles of the ANS have been shown to relate to posttraumatic stress disorder (PTSD; Chalmers et al., 2014; Sahar et al., 2001), cardiorespiratory, and gastrointestinal issues (Pacella et al., 2013). Empirical data shows that the exposure to traumatic events (direct or indirect, like learning or witnessing in person what happens to others), such as actual or threatened death, serious injury, or sexual violence (American Psychiatric Association, 2013)—affect the body and hinder the ability to cognitively process and verbally communicate the trau-matic event (Van der Kolk, 2014), especially if an event overwhelms a person’s ability to cope making fight/flight strategies ineffective, which determines trauma vulnerability (Poli et al., 2022; Van der Kolk et al., 2007). Thus, body psychotherapy (BPT) offers a promising approach working directly with processing somatic reactions and modulating dysregulated arousal (Langmuir et al., 2012; Ogden & Minton, 2000; Payne et al., 2015).
BPT: What Is It and How Is It Related to the Regulation of the ANS?
We will use the term body psychotherapy (BPT) in this article to refer to the group of psychotherapy modalities that primarily use body techniques in the therapeutic process, also labeled as somatic psychology, or body-oriented psychotherapy. Unlike other psycho-therapy modalities, BPT is primarily focused on direct work with the body, assuming its inseparable relationship with cognitive, emotional, perceptual, and physical aspects of self-experiences (Röhricht, 2009). The basic assumption in BPT is that emotional memories promote chronic or sensitized body reactions that influ-ence how we feel, move, and breathe. BPT shares some common features with other body–mind practices (e.g., yoga, tai chi, qi gong, etc.), such as work on breathing and attunement with body sensa-tions, while also incorporating thoughts and emotions. Unlike other body–mind practices, however, BPT follows the standards of psychotherapy, as a planned process with a clear theoretical back-ground and defined goals in the treatment of mental suffering or disorders. BPT particularly considers the therapeutic alliance, which is also acknowledged as recruiting the social engagement system (Porges, 2021), as one of the key elements of the healing process (Rosendahl et al., 2021). A recent meta-analysis confirmed that BPT is beneficial for a wide spectrum of psychic disorders (Rosendahl et al., 2021), including PTSD (van de Kamp et al., 2019).
Autonomic Reactivity and Body Awareness in BPT
Body awareness is the subjective experience that emerges from complex afferent (sensory) and efferent (motor) pathways and loops between different body parts and the central nervous system (Cameron, 2001; Craig, 2002; Gellhorn, 1964; Mandler et al., 1958; Mehling et al., 2009; Sherrington, 1906). Body awareness in BPT is considered as an inseparable aspect of embodied self-awareness in interaction with the environment (Mehling et al., 2011).
Sensitivity to internal body signals is more complex than simple quantity in terms of “more (or less) is better.” Empirical studies show that sensitized body awareness and somatosensory amplification are common in anxiety, panic attacks/disorder, and hypochondriasis (Cioffi,1991; Mehling et al., 2009). Attenuated/reduced perception of bodily signals is found in eating disorders (Herbert & Pollatos, 2012; Pollatos et al., 2007), while maladaptive rumination on intero-ceptive signals is noted in depression (Watkins & Teasdale, 2004). The ability to recognize subtle body signals may help managing fibromyalgia, chronic pain, or eating disorders (Daubenmier, 2005; Gard, 2005; Mehling et al., 2009, 2011). Thus, BPT is oriented on practicing body awareness characterized not by its intensity, but through specific attitudes and attentional focus (Fogel, 2009; Mehling et al., 2009).
Various meditation and body–mind practices provide multiple benefits, such as engaging the interoceptive network (Fox et al., 2016; Lutz et al., 2008), increasing vagal tone and dampening sympathetic activity (Brown & Gerbarg, 2005; Calabrese et al., 2000), and improving stress regulation and cognitive control (Sharma, 2014). It is important to note that unless persons with maltreatment history have prior work of identifying and developing coping skills (see, e.g., Van der Kolk, 2014), they may be threatened by increased body awareness. Meditation can trigger autonomic hyperarousal and traumatic memory reexperiencing (Van Dam et al., 2018). Nonethe-less, if applied properly, beneficial effects of those techniques on the ANS functioning are expected, and clinical practice and research studies show the beneficial effects of various body-oriented practices in working with trauma (Payne et al., 2015; Van der Kolk, 2014). Since training in BPT regularly includes personal therapy as a component of the training, a typical component of psychotherapy education in general (Moe & Thimm, 2021), such experiential training may reduce the link between maltreatment history and chronic body threat responses in (future) psychotherapists.
The Present Study
While it could be expected that BPT training and experience help BPT practitioners to regulate their ANS, to our knowledge, this specific population has not been previously studied. BPT practi-tioners typically have mixed backgrounds or receive training from eclectic BPT schools (Joki´c et al., 2019), similarly to psychothera-pists in other modalities (Cook et al., 2010). However, different meditation or body-oriented contemplative practices produce some similar responses, like stimulating the interoceptive network and insular cortex (Bonaz et al., 2021; Gibson, 2019). Thus, we sought to explore BPT practitioners as a specific group of psychotherapists who share the mutual key distinctions elaborated above, that is, understanding the body–mind relationship and applying BPT tech-niques in line with BPT praxis norms––which, as a result, may help BPT practitioners regulate their ANS.
The aim of this study was to identify whether BPT practitioners have fewer autonomic symptoms and a weaker link of ANS ymptoms with childhood maltreatment, compared to a general population. This is in line with past research showing that, compared to other professions, psychotherapists reported higher rates of adverse childhood experience but fewer mental problems and disturbances in adulthood (Elliott & Guy, 1993).
To test this, we used the Body Perception Questionnaire (BPQ; Porges, 1993; short form [BPQ-SF], Cabrera et al., 2018). Rooted in polyvagal theory, the BPQ is a self-report instrument that measures body experiences that emerge from the neurophysiologi-cal links between body and brain. Psychometric analyses of the BPQ in multiple samples revealed a single body awareness factor (which may reflect the shared afferent targets of cranial and spinal pathways in the brainstem), while autonomic reactivity is best described by subdiaphragmatic and supradiaphragmatic re-sponses––implying distinct efferent control systems that give rise to individual differences in physiological responses in separate parts of the body (Cabrera et al., 2018). Higher self-reported autonomic reactivity symptoms have been found to be associated with more severe trauma histories in general population samples (Kolacz, Dale, et al., 2020; Kolacz, Hu, et al., 2020), as well as less flexible regulation of the ventral vagal parasympathetic system and the sympathetic nervous system (Kolacz et al., 2022). However, psychometric studies have largely been conducted in general populations (e.g., Cabrera et al., 2018; Poli et al., 2021). Given that BPT training may affect sensitivity and attention to body sensations, a different factor structure of BPQ among BPT practi-tioners is possible.
Sensitivity analyses showed that the observed interaction between childhood maltreatment and sample membership remains, even when considering only U.S. body psychotherapists. On a related note, the general population data were collected before the COVID-19 pandemic, while the majority of BPT practitioners (70%) com-pleted the questionnaire after March 11, 2020, when the World Health Organization labeled the outbreak as a pandemic. However, it would be plausible to expect that autonomic symptoms in the BPT sample would be higher after the onset of the pandemic than in the prepandemic––meaning that the effects obtained in our present study would be even higher had we collected data from both samples at the same time. Future studies could include control data regarding symptoms of anxiety and depression to produce more robust results.
A limitation of the present study is that BPT practitioners were not compared to psychotherapists from different psychotherapy modalities. While most psychotherapists have mixed backgrounds combining training from various modalities (Cook et al., 2010), it would be relevant to compare two groups who significantly differ in experience with purely verbal versus dominantly body-related modalities. All face-to-face communication includes nonverbal cues, but intensive engagement in nonverbal interactions could promote higher levels of changes in autonomic reactivity. In addi-tion, we did not collect information on therapy experiences or use of body-based practice use in the general sample.
Another limitation is that we assessed body awareness and autonomic reactivity using a self-report measure, which relies on the frequency with which people are aware of or bothered by signals coming from within the body. To gain a better understanding of the relationship between body perception and practicing BPT, it would be important to also include some objective/sensor-based measures of the latter (such as heart rate variability or blood pressure). It is, for example, possible that BPT practitioners experience higher levels of arousal, or more frequent signals from within the body, but have learned to regulate arousal by how they pay attention to the signals, or even by ignoring them.
A methodological limitation is our measurement of years of practicing BPT with the category “9 or more years,” which included a significant number of participants who were excluded from analysis. Although we expected that the first years of practicing BPT (after training to become a psychotherapist) might be crucial for experiencing changes, examining a higher range of professional (body) psychotherapy experience might be insightful.
Further, follow-up studies with longitudinal data are needed to better understand the time course of changes in autonomic reactivity with BPT training. Finally, those who are less affected by their early maltreatment, or those who successfully recover, may be more likely to train to become psychotherapists or body psychotherapists, and to remain in the field. Since we analyzed single time point data, we were not able to corelate the timing of becoming a BPT with and having good autonomic regulation.
Conclusion
The BPQ-SF has consistent psychometrics within a sample of body psychotherapists compared to prior studies in general samples, which support its use as a tool for measuring body awareness and autonomic reactivity––even in those who have advanced training in noticing body sensations. Body psychotherapists reported higher rates of childhood maltreatment, but fewer symptoms related to autonomic functioning, and better differentiation of aspects of body awareness and autonomic reactivity than general populations, indi-cating possible beneficial effects of BPT training on adult ANS functioning. Successful BPT requires neural exercises that may enable the social engagement system to work in a coregulatory manner. This implies that body psychotherapists might be able to mediate the neuroception of threat signals (Porges, 2004), and offer cues of coregulation in voice, gesture, and facial expression to foster effective ANS regulation (shifts toward mobilization or calm as needed) in their clients.