Childhood Maltreatment Influences Autonomic Regulation and Mental Health in College Students
Childhood maltreatment history may influence autonomic reactivity and recovery to stressors. Hypothetically, the maltreatment history may contribute to a retuned autonomic nervous system that is reflected in a novel metric, vagal efficiency (VE), designed to assess the functional efficiency of vagal cardioinhibitory pathways on heart rate.
We explored whether VE mediates the well-documented relationship between maltreatment history and psychiatric symptoms. We also investigated the relationship between measures of autonomic regulation in response to the physical and emotional challenges and psychiatric symptoms. Participants (n = 167) completed self-report measures of psychiatric symptoms and had continuous beat-to-beat heart rate monitored before, during, and after physical and emotional stressors. Participants with maltreatment histories exhibited lower VE, which mediated the association of maltreatment history and the psychiatric symptoms of anxiety and depression. Consistent with prior literature, there were significant associations between maltreatment history and autonomic reactivity (i.e., heart rate and respiratory sinus arrhythmia) during emotional and physical challenges; however, when VE was entered as a covariate these associations were no longer statistically significant. Blunted VE may reflect a neural pathway through which maltreatment retunes autonomic regulation and provides a neurophysiological platform that increases mental health risk.
INTRODUCTION : Exposure to traumatic events may have psychological and physiological consequences that may be a result of dysregulation of the autonomic nervous system. Survivors of maltreatment, even those who do not reach the diagnostic criteria for PTSD, may have psychiatric and physical health features that relate to an autonomic nervous system that has been retuned to have a lower threshold to react to cues of threat (1–4). Prior research has shown that female college students with maltreatment histories, who did not reach the diagnostic criterion for PTSD, experienced more psychiatric symptoms, had lower levels of respiratory sinus arrythmia (RSA) and faster heart rates as demonstrated by their shorter heart periods (HP), and reacted di erently to the physical stressor of riding a stationary bike and the emotional stressor of watching a video of a child being maltreated than women without maltreatment histories (5, 6).
Additionally, meta-analyses found major depression and anxiety disorders such as panic disorder, PTSD, generalized anxiety disorder, and social anxiety are associated with lower heart rate variability (HRV)(7, 8). These patterns of autonomic reactivity and recovery to stressors might relate to atypical vagal regulation of the heart reflected in ineÿcient cardiohibitory vagal pathways (i.e., vagal brake) (6). Polyvagal Theory (9, 10) proposes that these protective responses spontaneously emerge through neuroception, a reflexive adaptive process that triggers specific biobehavioral response patterns to cope with conditions of safety, danger, and life threat. If neuroception detects safety, the nervous system facilitates social communication and engagement. In contrast, if neuroception detects danger, the withdrawal of the parasympathetic system may be initiated, reducing the impact of cardioinhibitory vagal pathways on the heart to functionally diminish the influence of the vagal brake on the heart’s pacemaker and increase access to greater metabolic resources in preparation for the challenge.
Following a successful response to the challenge, the parasympathetic nervous system initiates recovery by re-engaging the vagal brake to slow heart rate by increasing the cardioinhibitory actions of the vagus, while simultaneously inhibiting the sympathetic control of the heart (11, 12). Since the early 1900s, it had been known that the cardioinhibitory function of the vagus was systematically influenced by respiration (13). This observation is the physiological basis for quantifying the amplitude of the oscillation in heart rate at the frequency of spontaneous breathing, as an index of cardiac vagal tone (14). Lower levels of RSA have been associated with a greater sensitivity to unpredictable threat (15), a finding that relates to neuroception and has implications for individuals with a history of maltreatment. In this study, we explored this plausible explanation using vagal eÿciency (VE), a metric proposed by Porges and colleagues (16) as a measure of the dynamic regulation of cardiac vagal tone on cardiac output represented in a single measure of slope between sequential measures of HP and RSA.
We examined VE during the physical challenge of riding a stationary bike because it provided a physiological challenge with minimal potential psychological associations. In addition, the metabolic demands of biking require a systematic withdrawal of the vagal cardioinhibitory influence on the heart’s pacemaker (i.e., vagal brake), while the post-biking recovery enables the vagal brake to re-engage to slow heart rate. If the heart rate is tightly coupled and eÿciently driven by the vagal brake (i.e., measured by RSA), the linear regression between short (e.g., 15s) sequential estimates of RSA and heart rate will have a steep slope. Although no published studies have examined how VE relates to maltreatment history and psychiatric symptoms, it is important to consider VE as it may be developmentally sensitive to environmental conditions. In preterm infants, VE has been found to increase with maturation and to be influenced by a psychosocial intervention (17).
Furthermore, its sensitivity to environmental conditions was demonstrated as VE was reliably reduced following the administration of alcohol in adults (18). VE may also predict intervention response, with evidence showing that adolescents with low VE were more responsive to neurostimulation for their gastric pain than those whose VE was high (19). Consistent with Polyvagal Theory (9–11, 20, 21), which emphasizes the mediational role of autonomic state as an intervening variable, it is important to investigate autonomic reactions to an emotional stressor because exposure to traumatic events may retune autonomic regulation and contribute to dysfunctional emotional processing (22, 23).
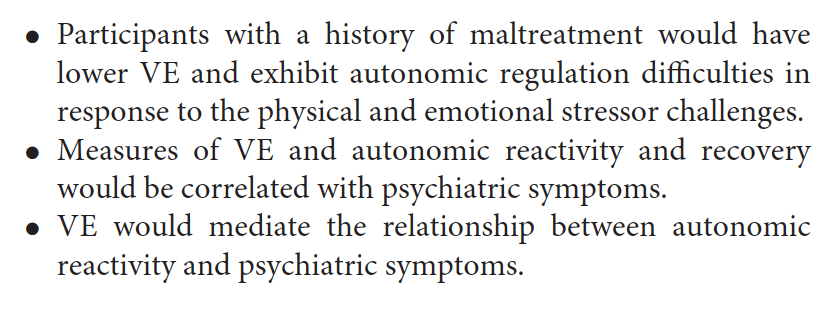
These individuals may adaptably become hypervigilant for danger cues and have anticipatory or responsive physiological changes in their autonomic nervous system that promote defensive action and may influence psychological wellbeing. When confronted with emotional challenges, including emotional imagery and emotional scene viewing, individuals exposed to stressful events have consistently showed atypical physiological and neural responses (24–29). We also investigated autonomic responses during the emotional stressor of watching a video of a child being maltreated and contrasted it to the reaction during the physical stressor. The current study explored whether VE was reduced in those with a maltreatment history, and whether it mediated the relationship between maltreatment history and psychiatric symptoms (i.e., somatization, anxiety, depression, and PTSD). We also investigated whether VE mediated the relationship between measures of autonomic regulation in response to the physical and emotional challenges and psychiatric symptoms. We hypothesized that:
MATERIALS AND METHODS
Participants
Participants were 167 college students (65.9% identified as female), recruited from a university’s participant pool for two separate studies, who had data for all the physiological measures. They were 18–25 years old (M = 19.18, SD = 1.33), predominantly first-year (45.5%) or second year (25.7%) students. The racially diverse sample identified themselves as White (43.7%), Black (16.8%), Hispanic (9.0%), Asian/Pacific Islander (6.0%), and mixed/other (24.6%). Those reporting a medical diagnosis (8.4%) did not report having a cardiovascular disorder, which would have excluded them from participation in this study.
Participants with a prior psychiatric diagnosis (25.1%) most frequently reported having anxiety (15.6%), depression (14.4%), ADHD (8.4%), and PTSD (2.4%). There were no participants that did not endorse at least mild maltreatment for at least one of the items. Many reported experiencing moderate or severe childhood maltreatment (48.5%) including emotional neglect (31.1%), emotional abuse (28.1%), physical neglect (18.6%), physical abuse (16.8%), and sexual abuse (13.2%). Participants varied in their current symptomatology (non-windsorized values for somatization M = 3.27, SD = 4.01; depression M = 4.57, SD = 5.07; anxiety M = 4.93, SD = 5.14; and PTSD M = 30.33, SD = 10.49) and those reporting more of one symptom reported more of another (correlations ranged 0.52–0.75, p < 0.001).
Procedure
The university’s Institutional Review Board approved all procedures. During the data collection sessions, the participant was provided with an informed consent form explaining the voluntary nature and purpose of the study, participation requirements, and confidentiality and privacy procedures. Each participant was informed there were no known physical or psychological risks from participating in this study and that the investigator should be notified if they were distressed. Once written consent was obtained, the participant completed self-report measures with the least sensitive/personal information being asked first and the most sensitive/personal information last. Then the participant was asked their height and weight and instructed on how to attach the electrodes for the heart rate monitoring. All participants were first exposed to the physical stressor of riding the stationary bike at a comfortable pace for half a mile (usually 2–4 min) and then the emotional stressor of watching a video in which a child is emotionally maltreated (3 min). Data were collected during a 3-min baseline prior to and after each stressor to enable the quantification of changes in heart rate and respiratory sinus arrhythmia to the experimental challenges.
As a precaution, the instruments assessing symptoms of depression and PTSD were scored immediately to determine if the participant reported having in the past 7 days any desire to end their life and being extremely hopeless about the future and endorsed a clinically significant level of traumatic stress (scored 44 or higher on the measure of PTSD symptomatology). This protocol identified about 30%of the participants that needed an immediate assessment to determine level of risk by the licensed clinical psychologist that was part of the research team. All participants were referred to the counseling center and provided with an information sheet that explained other relevant university services (e.g., academic support services). Because none of these participants required psychiatric hospitalization, they all remained in the study. After data collection, participants were provided with a debriefing form that had information about the study and resources on campus.
Constructs and Measures
Maltreatment history was assessed via the Childhood Trauma Questionnaire (30), which is a 28-item self-report questionnaire that asks adolescents and adults about how often they experienced emotional abuse, sexual abuse, physical abuse, emotional neglect, and physical neglect. This measure is internally consistent (α = 0.66–0.93), reliable (test-retest r = 0.86), and converges with corroborated clinician reports of maltreatment history (31, 32). A binary childhood maltreatment score was derived by determining if the individual reported moderate or severe maltreatment in any of the five domains.
Psychiatric symptoms were assessed via two measures. Depression, anxiety, and somatization symptoms were assessed via the 18-item version of the Brief Symptom Inventory (33), which asks participants to indicate via a 5-point Likert scale (not at all to extremely) how much they have been distressed or bothered in the past 7 days by each symptom. Reliability analyses indicated that the measure was internally consistent with the current sample (Cronbach’s alpha scores somatization = 0.81; anxiety = 0.87, and depression = 0.88).
PTSD symptoms were assessed via the PTSD Checklist—Civilian Version (34), a 17-item self-report measure that corresponds to the criteria for PTSD and assesses via a 5-point Likert scale (not at all to extremely) level of distress related to stressful life experiences over the last month. This measure has good convergent and discriminant validity, internal consistency, and test–retest reliability (35) and was found to be internally consistent with the current sample (Cronbach’s alpha = 0.92).
Physiological data were monitored with an EZ-IBI monitor (UFI, Morro Bay, CA). Two active electrodes were placed on the left side at the level of the heart and on the right lower abdomen. A ground electrode was placed above the right-side collarbone. ECG data was collected continuously while the participant went through the protocol. The EZ-IBI detected the peak of the R-wave with 1-ms accuracy (sampling rate = 1,000 Hz) and timed the interval ms between sequential R-R waves (i.e., heart period, HP), which were downloaded to a computer for o -line processing and analyses. Files of sequential HP were stored on a computer. HP was used as the metric of heart rate (i.e., HP is monotonically related to heart rate).
Quantification of heart rate variability requires the timing of intervals between successive heart beats synchronized with successive peaks of the R-wave in the ECG. In this paper, we label the R-R intervals defining interbeat intervals, as heart period. We elected to report the data using heart period instead of heart rate because heart period reflects a stronger linear relationship than heart rate with dynamic vagal influences (36).
RSA estimates calculated based on the methods developed by Porges (37) included the following procedures: (a) the R-R interval time series were converted to time-based data by resampling at successive 500-ms intervals; (b) a 21-point moving cubic polynomial filter was stepped through the time-sampled series to produce a smoothed template series; (c) the template series was subtracted from the original series to produce a residual time series; (d) the residual time series was processed by a digital bandpass filter with 25
coeÿcients to extract the variance in the frequency band of 0.12–0.40 Hz (i.e., frequency of spontaneous breathing for adults); and (e) bandpassed variance was transformed to its natural logarithm and used to quantify RSA. These procedures result in a sensitive, non-invasive marker of the influence of the myelinated vagal fibers on the heart (9, 11, 13, 38).
Data files were input into CardioEdit software (39) to visually display sequential R-R interval data and edit outliers. Edited data were processed with CardioBatch software (39) to generate measures of mean 30-s epochs for HP and RSA.
Baseline levels were based on the first segment collected. Autonomic metrics reflected the magnitude of change in RSA and HP from baseline to stressor (reactivity) and stressor to post-stressor (recovery) for the physical and emotional stressors. Reactivity change scores were calculated by subtracting the value during the pre-stressor baseline from the value during the stressor. Recovery change scores were calculated by subtracting the value during the stressor from the value during the post-stressor recovery period. VE was used to measure cardiac autonomic regulation, specifically how vagal e erent pathways to the heart dynamically
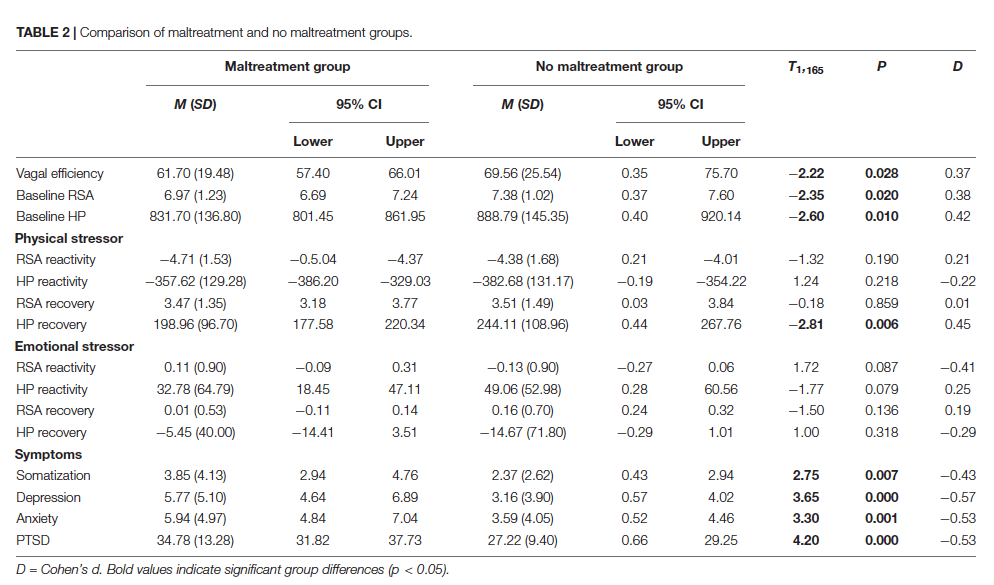
D = Cohen’s d. Bold values indicate significant group differences (p < 0.05).
influences heart rate, which is a process that is not captured in RSA alone (19). Following methods from prior studies (19, 40), VE was calculated for each participant as the slope of the regression line between RSA and HP using paired sequential epoch values (every 15 s) of HP and RSA during the physical challenge (i.e., 3-min baseline, riding the stationary bike, and post-biking recovery).
Statistical Analysis
Data analyses were conducted in SSPS and R. To retain participants and minimize the e ects of symptomatology outliers, a 90% windsorization procedure was used. Correlational analyses explored the relationship among the autonomic measures (i.e., VE, baseline levels and changes in RSA and HP in response to physical and emotional stressors) and psychiatric symptomatology. Independent sample t-tests compared participant groups with and without self-reported history of maltreatment.
Mediation analyses, conducted using the Lavaan R package (41), assessed whether the association between the independent variable of maltreatment history (yes/no) and dependent variables of psychiatric symptoms could be attributed to the indirect e ect of the third variable of VE. For this analysis, the indirect e ect, which represents the strength of the mediation, is the product of the coeÿcient of the independent variable on the mediator and the mediator on the outcome variable and the direct e ect is the e ect of the independent variable on the dependent variable adjusting for the e ect of the mediator. Mediation models were estimated using maximum likelihood. Indirect and total e ect confidence intervals were calculated *p < 0.05, **p < 0.01.
using bias-corrected adjusted bootstrap percentiles with 10,000 draws, which has superior power for detecting true e ects with accurate Type I error rates compared to other methods (42). Mediation was supported if the indirect e ect 95% confidence interval did not include zero.
The final analyses did not focus on maltreatment history. Instead, the repeated measures analyses explored whether participants who scored above and below the clinical cuto scores for somatization, depression, anxiety, and PTSD symptoms varied in their HP changes during the physical and emotional stressor challenges. We also explored whether these e ects remained when VE was entered as a covariate.
RESULTS
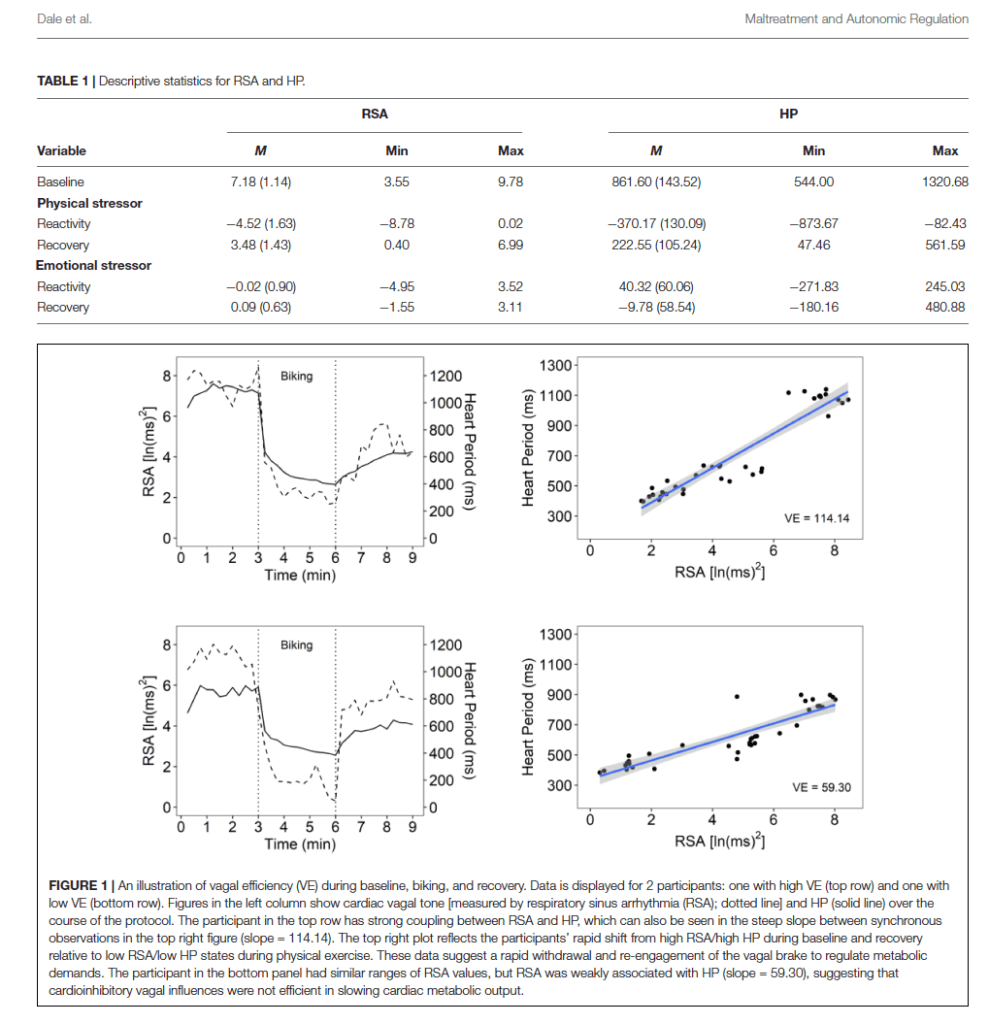
Distributions of the autonomic variables (i.e., VE, HP, and RSA) were explored for outliers. One extreme outlier on the VE measure (VE = 280.99, 6 SD above mean) was removed from the analysis. With this exclusion, VE scores ranged from 22.37 to 158.61 (M = 66.06, SD = 23.38). Table 1 provides the descriptive statistics for the baseline and changes scores [natural log (ln) units for RSA and ms for HP].
Vagal Efficiency
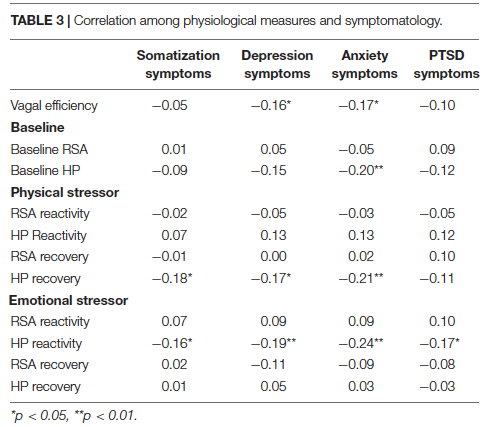
Figure 1 illustrates VE for a participant with high VE and one with low VE. Table 2 documents that participants with a maltreatment history exhibited dampened autonomic regulation reflected in lower RSA and HP baseline measures and lower VE. In addition, the participants with a maltreatment history reported more psychiatric symptoms.
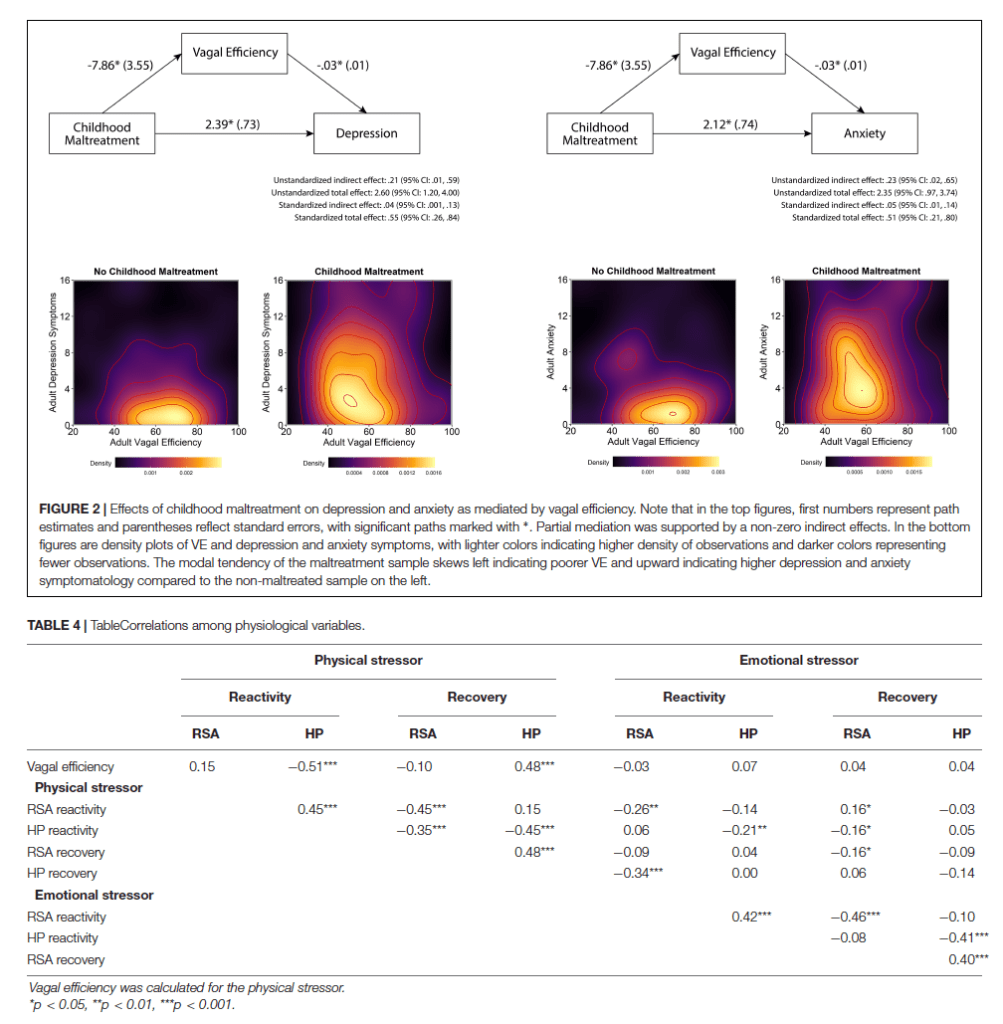
Independent of maltreatment history, participants with lower VE reported more symptoms of depression and anxiety (Table 3). As illustrated in Figure 2, mediation analyses assessing whether the association between maltreatment history and the symptoms of depression and anxiety could be attributed to VE found evidence of partial mediation for both depression and anxiety. The indirect e ect in both models was significant, with childhood maltreatment history being associated with lower VE, which—in turn—was associated with higher levels of anxiety and depression symptoms (Figure 2 top panels). Plots of raw distributions showed that participants with childhood maltreatment had higher scores in adult depressive symptoms and adult anxiety that were associated with lower VE. This was in contrast to participants without childhood maltreatment history who had higher VE and concurrently lower levels of anxiety and depression symptoms (Figure 2 bottom panels).
Maltreatment History, ANS Regulation, and Symptomatology
As reported in Table 4, VE was correlated with baseline levels, and HP reactivity and recovery to the physical stressor. The negative correlation between VE and HP reactivity indicates that participants with higher VE exhibited a greater reduction in HP in response to the physical stressor, which suggests greater increases in heart rate. Whereas, the positive correlation between VE and HP recovery indicates that participants with higher VE exhibited a greater increase in HP after the physical stressor, which suggests greater slowing of their heart rates.
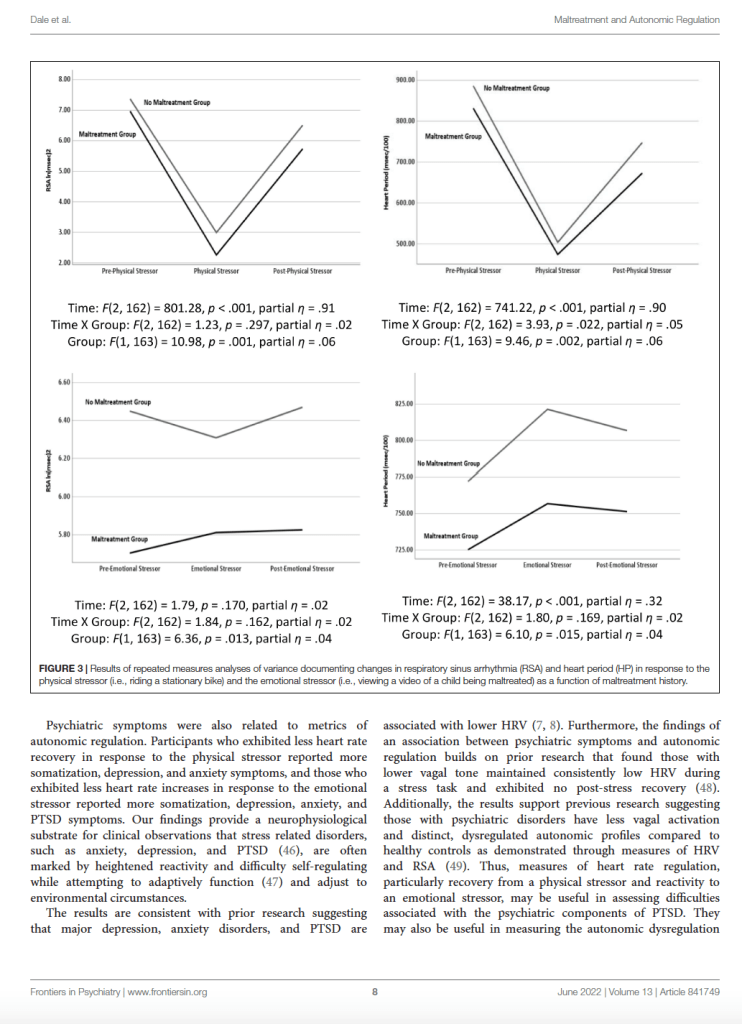
As illustrated in Figure 3, the repeated measures were significantly di erent during the physical challenge for RSA and HP. During the emotional challenge, only HP systematically changed during the protocol. Note in the figure the significant between group di erences with the maltreatment group having consistently lower levels of RSA and HP. In addition, a significant maltreatment group X repeated measures interaction documented that the HP reaction during the physical challenge significantly di ered between the groups. As reported in Table 2, the participants with histories of maltreatment exhibited significantly less HP recovery in response to the physical stressor and less RSA reactivity in response to the emotional stressor.
As reported in Table 3, only measures of HP reactivity and recovery were associated with psychiatric symptoms. Participants with lower baseline HP levels reported more anxiety and PTSD symptoms; less HP recovery from the physical stressor reported more somatization, depression, and anxiety symptoms; and less HP reactivity in response to the emotional stressor reported more somatization, depression, anxiety, and PTSD symptoms. However, consistent with the mediation analyses, when VE was included as a covariate most correlations were no longer significant. The only remaining significant relationships were between HP recovery to the physical stressor and anxiety symptoms (r = −0.25, p = 0.027) and HP reactivity to the physical stressor and anxiety and PTSD symptoms (r = 0.23, p = 0.042 and r = 0.35, p = 0.002).
Exploring Pathways of Mediation
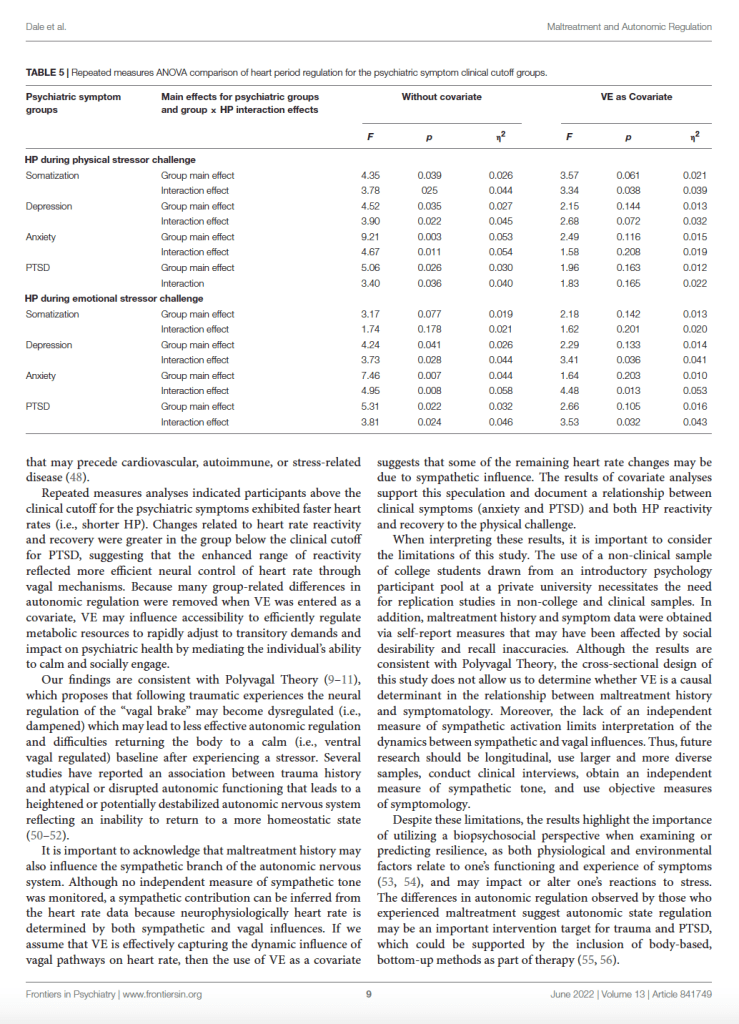
Table 5 displays the results of repeated measures analyses exploring whether participants who scored above and below the clinical cuto scores for somatization, depression, anxiety, and PTSD symptoms varied in their HP changes during the physical and emotional stressor challenges. Specifically, we looked for main e ects related to group status and interaction e ects that considered the interaction of group status and HP levels. We also explored whether these e ects remained when VE was entered as a covariate. As evident in Table 5, participants scoring above and below the clinical cuto s for psychiatric symptomatology di ered in the HP response to the physical and emotional stressor challenges. When VE was used as a covariate in analyses evaluating the autonomic responses to the physical stressor challenge for groups defined as above or below the clinical cuto s for somatization, depression, anxiety, and PTSD the observed clinically related shorter HP was no longer statistically significant. In addition, for the groups defined by being below and above the clinical cuto s for somatization, depression, anxiety, and PTSD there were significant group by repeated measures interactions. When VE was included as a covariate, the only significant interaction that remained was between the somatization groups. Similarly, with the emotional stressor challenge, the significant group di erences related to depression, anxiety, and PTSD symptomatology were no longer present when VE was entered as a covariate. However, entering of VE as a covariate did not impact the HP by group interaction e ects for the depression, anxiety, and PTSD groups (Table 5).
DISCUSSION
In this study, we expanded prior research (6) that documented that maltreatment history was associated with ineÿcient or atypical vagal regulation of the heart in response to physical and emotional stressors. In this study, we investigated whether these findings relate to di erences in VE. Consistent with our hypothesis, we documented that a history of maltreatment was related to lower levels of VE and that VE was related to dampened heart rate reactivity and recovery to the physical stressor.
Further support comes from the finding that participants with lower VE levels reported more depression and anxiety symptoms, and that VE mediated the relationship between maltreatment history and depression and anxiety symptoms. These findings are consistent with Polyvagal Theory (9–11, 20, 21), which proposes that autonomic state functions as an intervening variable mediating reactivity to challenges. The findings are also consistent with prior research (43) that documented that a subjective measure of autonomic reactivity (i.e., Body Perception Questionnaire) (44, 45) mediated the relationship between maltreatment history and current worry, depression, and PTSD symptoms during the pandemic. Future research will need to address whether subjective experiences of autonomic symptoms positively correspond with sensor-based measures such as VE.














Responses